Understanding Varicose Veins: Causes, Symptoms, and Treatments
May 31, 2023Varicose veins are a common vascular condition that affects lot of people all over the world. These enlarged, twisted veins, most frequently found in the legs, cause pain, and aesthetic concerns. Varicose veins are often considered a cosmetic issue, they can cause more serious health problems if they are untreated. This article aims to offer an in-depth understanding of varicose veins, including the causes, symptoms, and treatment options.
What are Varicose Veins?
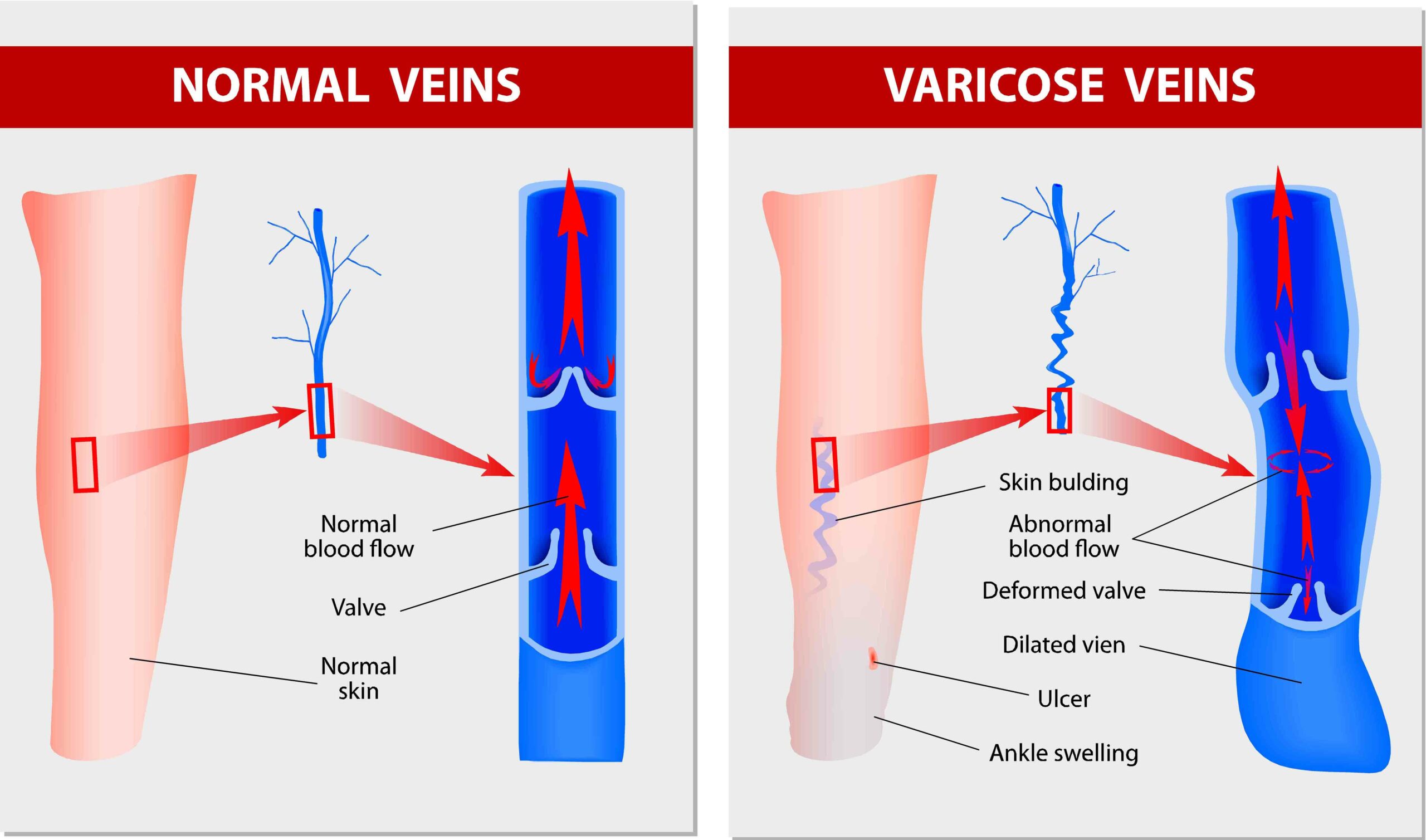
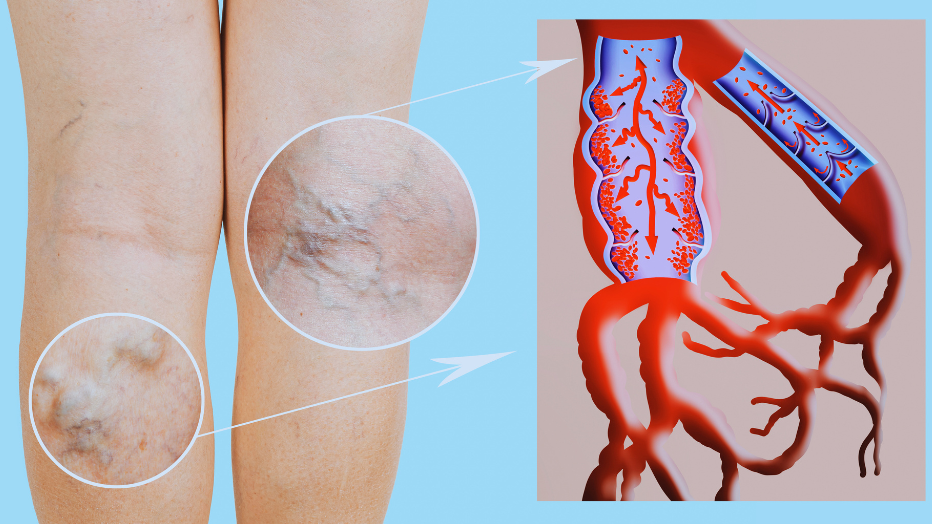
Varicose veins are veins that have become dilated, elongated, and twisted. They usually occur in the superficial veins of the legs, where they are more visible. Varicose veins develop when the valves within the veins damaged or veaken, leading to poor blood flow and the accumulation of blood within the veins.
Causes of Varicose Veins
Several factors add to the development of varicose veins. Some of the most common causes are the following ones:
- Age: As we are getting older, the elasticity of the veins reduces, making them more prone to dilation and the development of varicose veins.
- Genetics: Family history plays a significant role in determining an individual’s susceptibility to varicose veins. If your close relatives have varicose veins, there is a higher chance you will have too.
- Gender: Women are more likely to have varicose veins than men. Hormonal changes during pregnancy and menopause can increase the risk.
- Long-term sitting or standing: Professions that require long periods of standing or sitting without any movement can lead to impaired blood circulation and the development of varicose veins.
- Overweight: Excess weight places additional pressure on the veins, increasing the probability of venous insufficiency and the development of varicose veins.
- Lifestyle: Absence of regular exercise, smoking, and a sedentary lifestyle can assist in poor circulation and the formation of varicose veins.
Unveiling the Symptoms of Varicose Veins: Recognizing the Warning Signs
Introduction
Varicose veins, though commonly considered a cosmetic concern, can be evident a range of symptoms that impact daily life and overall health. Recognizing the symptoms of varicose veins is essential for early detection, proper diagnosis, and timely intervention. This article aims to shed light on the various symptoms associated with varicose veins, empowering individuals to seek appropriate medical attention and explore available treatment options.
Visible Veins: Twisted, Bulging, and Discolored
The most obvious and recognizable symptom of varicose veins is the visible appearance of enlarged, twisted, and lusty veins on the surface of the skin. These veins typically have a dark purple or blue colour, noticeably contrasting with the adjacent skin. They might appear rope-like or twisted, resembling raised cords.
Leg Discomfort and Pain
Varicose veins often cause discomfort and pain. The following perceptions and signs are often reported:
- Aching or pulsating: Individuals with varicose veins many times experience a persistent dull ache or throbbing sensation in the affected areas, typically the lower legs.
- Heaviness: The legs might feel heavy or tired, especially after prolonged periods of standing or sitting.
- Burning: Some people might experience a continuous burning sensation or itching around the affected veins, which can be aggravated by warm weather or standing for prolonged durations.
- Muscle cramps: Varicose veins might contribute to muscle cramps, specially at night, leading to discomfort and sleep disturbances.
- Restless legs syndrome (RLS): RLS is characterized by an irresistible urge to move the legs, commonly due to discomfort, tingling, or a crawling sensation. Varicose veins can exacerbate RLS symptoms.
Swelling and Edema
Varicose veins can cause fluid retention and swelling in the affected areas, most often in the lower legs and ankles. The swelling is commonly more pronounced after prolonged periods of inactivity or prolonged standing. The affected limb may feel heavy and appear visibly swollen.
Skin Changes and Complications
Gradually, varicose veins can cause skin-related symptoms and complications, like:
- Skin discoloration: The skin around varicose veins may darken or become discolored, often presenting as a reddish-brown or purplish hue. This occurs due to the accumulation of waste products and red blood cells leaking from the affected veins.
- Skin ulcers and sores: In severe cases, the constant accumulation of fluid and increased pressure in the affected veins can lead to the development of skin ulcers or sores. These ulcers usually form near the ankles and are slow to heal. They may be accompanied by pain and a risk of infection.
- Superficial thrombophlebitis: Varicose veins are susceptible to inflammation and blood clot formation, a condition known as superficial thrombophlebitis. This perharps present as a red, tender, and painful cord-like vein near the skin’s surface.
Resting Indicators and Aggravating Factors
- Worsening symptoms with prolonged sitting or standing: Varicose vein symptoms tend to worsen with long term sitting or standing. Inactivity can impede blood flow and exacerbate the pooling of blood in the veins, amplifying discomfort and visible symptoms.
- Relief with leg elevation: Elevating the legs above heart level can provide temporary relief from symptoms. By promoting blood flow and reducing venous pressure, elevation helps alleviate discomfort and pain associated with varicose veins.
If you suspect you have varicose veins, it’s important to consult a healthcare professional for an accurate diagnosis. During a physical examination, the doctor will examine your legs and ask about your symptoms. In some cases, additional tests may be conducted, like a Doppler ultrasound, to assess blood flow and identify any underlying venous insufficiency.
Exploring Treatment Options for Varicose Veins: Relieving Discomfort and Enhancing Vascular Health
Varicose veins, with their unsightly appearance and potential for discomfort, can significantly impact one’s quality of life. Fortunately, some treatment options are available to manage varicose veins, alleviate symptoms, and improve vascular health. In this article, we will explore various treatment modalities, ranging from conservative approaches to minimally invasive procedures, empowering individuals to make informed decisions about their varicose vein management.
Lifestyle Modifications and Self-Care
- Regular Exercise: Engaging in regular physical activity, like walking, swimming, or cycling, promotes healthy blood circulation, strengthens calf muscles, and helps alleviate symptoms associated with varicose veins.
- Weight Management: Maintaining a healthy weight reduces the pressure on the veins, decreasing the risk of varicose veins and relieving symptoms in those already affected.
- Elevation and Rest: Elevating the legs above heart level periodically throughout the day helps alleviate swelling and discomfort associated with varicose veins. Resting with legs elevated after prolonged standing or sitting is particularly beneficial.
- Compression Therapy: Wearing compression stockings or socks provides external pressure on the legs, promoting blood flow and reducing symptoms. Different compression levels are available, and your healthcare provider can recommend the best option.
Sclerotherapy
Sclerotherapy is a common non-surgical treatment option for varicose veins. During the procedure, a sclerosing agent is injected directly into the affected vein, causing it to collapse and seal shut. The body then absorbs the treated vein, redirecting blood flow to healthier veins. Sclerotherapy is effective for smaller varicose veins and spider veins.
Endovenous Laser Ablation (EVLA)
Endovenous laser ablation (EVLT), involves the use of laser energy to seal off and collapse varicose veins. A small fiber is inserted into the vein, and laser energy is applied, causing the vein to close. Blood flow is rerouted to healthier veins, reducing symptoms and improving overall vascular health. EVLA is a minimally invasive procedure performed under local anesthesia.
Radiofrequency Ablation (RFA)
Radiofrequency ablation is another minimally invasive treatment option for varicose veins. It involves the use of radiofrequency energy to heat and close off the affected vein. A catheter is inserted into the vein, delivering controlled heat energy, which causes the vein to collapse and seal. RFA offers a really safe and effective alternative to surgical vein stripping.
Glue ablation
Glue ablation, also known as venous closure with glue, is a minimally invasive procedure used in vascular surgery to treat varicose veins. It involves injecting a special medical adhesive into the affected vein, which seals it shut. This method promotes the redirection of blood flow to healthier veins, relieving symptoms and improving overall venous function.
Vein Stripping and Ligation
Vein stripping and ligation are traditional surgical procedures that are now less common due to the availability of less invasive alternatives. Vein stripping involves the removal of the affected vein through small incisions. Ligation involves tying off the vein to redirect blood flow to healthier veins. These surgical interventions may be considered in more severe cases or if other treatment options have been ineffective.
Ambulatory Phlebectomy
Ambulatory phlebectomy is a minimally invasive surgical procedure suitable for larger varicose veins close to the skin’s surface. Small incisions are made along the affected vein, and the vein is removed in sections using a special hook. This procedure is performed on an outpatient basis and requires local anesthesia.
Combined Treatment Approaches
Sometimes a combination of treatments may be recommended to address varicose veins comprehensively. For example, sclerotherapy may be used in conjunction with minimally invasive procedures like EVLA or RFA to target both smaller and larger veins, achieving optimal results.
