Blood clots: symptoms, risks, and prevention tips
August 15, 2024Blood clots, or thrombi, form in veins or arteries to prevent excessive bleeding but can cause serious health issues when they form inappropriately. They can obstruct blood flow, leading to conditions such as deep vein thrombosis (DVT), pulmonary embolism (PE), and strokes. Recognizing the symptoms and understanding the risks associated with blood clots is crucial for timely medical intervention.
Early detection and treatment are essential to reduce the risk of severe complications. Additionally, being informed about preventive measures can help individuals adopt healthier lifestyles and lower their risk of developing blood clots. This article provides insights into blood clot symptoms, risks, and effective prevention tips to help readers stay proactive about their health.
What are blood clots?
Blood clots, or thrombi, are masses of blood that transition from a liquid to a gel-like state. This transformation is part of a natural process called blood clotting, which is essential for stopping bleeding when blood vessels are injured. However, when blood clots form inappropriately within veins or arteries, they can obstruct blood flow and lead to serious health issues.
There are two primary types of blood clots:
- Arterial clots: These form in arteries that carry oxygen-rich blood away from the heart. They can lead to severe conditions like heart attacks and strokes by blocking blood flow to vital organs.
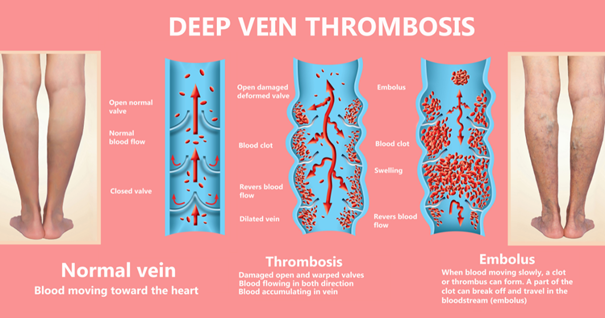
- Venous clots: These develop in veins that return deoxygenated blood back to the heart. Venous clots can cause deep vein thrombosis (DVT) and pulmonary embolism (PE), both of which can have serious health implications.
Understanding these types of blood clots and their formation processes is crucial for recognizing symptoms and seeking appropriate medical care. For more detailed information, you can visit resources such as the CDC’s page on venous thromboembolism.
Common symptoms of blood clots
Recognizing blood clot symptoms is crucial for early diagnosis and treatment. Symptoms can vary depending on the clot’s location:
Deep Vein Thrombosis (DVT)
Blood clot symptoms associated with DVT include:
- Swelling in one leg
- Pain or tenderness in the leg, often resembling a cramp
- Red or discolored skin on the leg
- Warmth in the affected leg
Pulmonary Embolism (PE)
Symptoms of PE, a serious condition where a clot travels to the lungs, include:
- Sudden shortness of breath
- Sharp chest pain, worsening with deep breaths
- Rapid heart rate
- Coughing up blood
- Lightheadedness or fainting
Other potential symptoms based on clot location
- Early stage blood clot in leg symptoms: Mild ache or discomfort in the calf or thigh in addition to DVT symptoms.
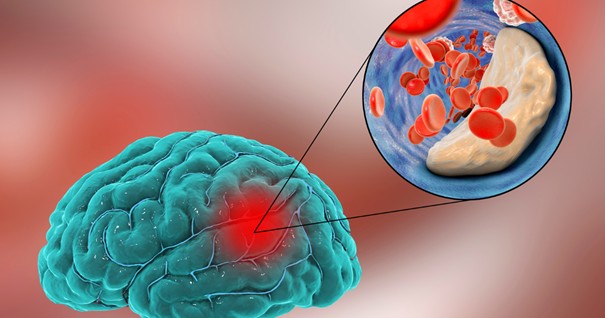
- Brain blood clot symptoms: Sudden severe headache, confusion, difficulty speaking, vision problems, and weakness or numbness on one side of the body.
Risk factors for developing blood clots
Understanding the risk factors for developing blood clots is essential for prevention and early intervention.
Genetic predispositions
- Hereditary conditions like Factor V Leiden or Prothrombin gene mutations increase the risk of abnormal blood clotting.
- Family history of blood clots is crucial for assessing personal risk.
Lifestyle and environmental factors
- Prolonged immobility (e.g., long flights, bed rest) hinders blood flow, leading to clot formation.
- Smoking, lack of physical activity, and obesity elevate the risk of developing blood clots.
- Maintaining a healthy weight, staying active, and avoiding smoking are key preventive measures.
Medical conditions and surgeries
- Conditions like cancer, heart disease, and inflammatory diseases increase blood clotting tendencies.
- Surgeries, especially involving the hips, legs, or abdomen, heighten the risk.
- Recognizing blood clot symptoms post-surgery, such as unusual swelling or pain, is vital for timely medical evaluation.
Diagnosing blood clots
Accurate diagnosis of blood clots is crucial for timely and effective treatment.
Common diagnostic tests and procedures
- Ultrasound imaging: Visualizes blood flow and identifies clots, particularly in suspected DVT cases.
- CT or V/Q scans: Used to examine the lungs for pulmonary embolism (PE).
- D-dimer blood tests: Measure a substance released when a blood clot breaks up, indicating clot formation.
Importance of early detection
- Early detection prevents serious complications.
- Recognizing blood clot symptoms like swelling, pain, redness in the legs, or sudden shortness of breath and chest pain can lead to prompt intervention and better outcomes.
A thorough medical history and physical examination play a vital role in diagnosing blood clots. Physicians will inquire about personal and family history of blood clots, lifestyle factors, recent surgeries, and any underlying medical conditions. During the physical examination, they will look for signs of blood clot symptoms, such as swelling, tenderness, or discoloration in the affected area. This comprehensive approach ensures that all potential risk factors and symptoms are considered in the diagnostic process.
By using these diagnostic methods and emphasizing early detection, healthcare providers can effectively diagnose blood clots and implement appropriate treatment strategies.
Potential complications of blood clots
Blood clots can cause serious short-term and long-term health complications.
Short-term and Long-term Health Impacts
- Short-term: A blood clot can cause immediate issues like pain, swelling, and discomfort in the leg (DVT). If a clot travels to the lungs (PE), it can cause difficulty breathing, chest pain, and rapid heart rate.
- Long-term: Untreated blood clots can lead to chronic conditions such as post-thrombotic syndrome, causing persistent pain and swelling. A blood clot in the brain can lead to stroke, resulting in brain blood clot symptoms like severe headache, confusion, and impaired motor functions.
Untreated clots can grow and block blood flow, damaging tissue, and organs. Pulmonary embolism can cause sudden death, while a stroke can result in permanent disability or death. Prompt treatment is crucial.
Blood clots are often associated with other underlying health conditions, which can exacerbate their impact. For example, individuals with cardiovascular diseases, such as atrial fibrillation, are at a higher risk of forming blood clots that can lead to stroke. Cancer patients also have an elevated risk due to the prothrombotic state induced by malignancies and certain cancer treatments. Additionally, conditions like diabetes and obesity contribute to an increased likelihood of blood clot formation. Understanding these connections underscores the importance of comprehensive medical management to address both the blood clot and its associated health conditions.
Treatment options for blood clots
Effective blood clot treatment is crucial to prevent serious health complications. Treatment strategies vary based on the clot’s type, location, and severity.
Medications (Anticoagulants, Thrombolytics)
- Anticoagulants: Blood thinners like heparin, warfarin, and newer oral anticoagulants (rivaroxaban, apixaban) prevent new clots from forming and stop existing clots from growing. This is a primary method of blood clot treatment.
- Thrombolytics: Clot-busting drugs such as tissue plasminogen activator (tPA) are used in emergencies to rapidly dissolve life-threatening clots, particularly in cases of pulmonary embolism or stroke. These are vital components of blood clot treatment.
Surgical interventions
- Thrombectomy: Surgical removal of the clot from the blood vessel.
- Vena cava filter: Prevents clots from traveling to the lungs, used when medications are ineffective or when a clot poses an immediate threat to vital organs.
Non-surgical treatments
- Compression stockings: Improve blood flow in the legs and reduce swelling, especially for deep vein thrombosis (DVT) patients.
- Regular monitoring: Ensures blood clot treatment effectiveness and addresses any complications promptly.
Effective prevention strategies
Preventing blood clots is crucial for overall health and reducing the risk of serious complications.
Lifestyle modifications (diet, exercise)
- Regular exercise: Improves circulation, preventing blood from pooling.
- Balanced diet: Rich in fruits, vegetables, whole grains, and lean proteins supports cardiovascular health.
- Hydration: Staying hydrated prevents increased blood viscosity and clotting risks.
Tips for reducing risk during travel and sedentary periods
- Movement breaks: Regularly stand up and move to promote circulation.
- Simple exercises: Flex and extend ankles to keep blood flowing.
- Hydration: Drink plenty of water to avoid dehydration and clot formation.
- Compression stockings: Wear during travel if prone to early stage blood clot in leg symptoms.
- Avoid tight clothing and maintain good posture to reduce clotting risks.
Incorporating these strategies helps lower the risk of blood clots and supports better health.

When to seek medical help
Recognizing when to seek medical help for blood clots is crucial for preventing severe complications and ensuring timely treatment.
- Emergency signs: Sudden shortness of breath, sharp chest pain worsening with deep breathing, or rapid heart rate could indicate a pulmonary embolism.
- Brain clot symptoms: Sudden, severe headache, difficulty speaking, and vision problems may signal a brain clot leading to a stroke.
- DVT symptoms: Significant swelling, pain, or redness in the legs, especially with warmth, suggest deep vein thrombosis (DVT).
Guidelines for seeking professional advice
- Contact your healthcare provider if you experience ongoing pain, swelling, or discoloration in your limbs, which may be blood clot symptoms.
- Unexplained shortness of breath, chest pain, or lightheadedness should prompt an immediate visit to the emergency room.
Regular check-ups and monitoring play a vital role in preventing blood clots, especially for individuals with a history of clotting disorders or other risk factors. Routine medical appointments allow healthcare providers to assess your risk, monitor any symptoms, and adjust preventive strategies as needed. If you have been diagnosed with a blood clot previously, consistent follow-up care is crucial to ensure effective management and to prevent recurrence. Maintaining open communication with your healthcare provider about any new or worsening blood clot symptoms is essential for ongoing health and safety.
Recognizing symptoms early, seeking timely medical advice, and adhering to regular check-ups can effectively manage the risk of blood clots and maintain better overall health.
Blood clots are a serious medical condition that can lead to severe health complications if not promptly diagnosed and treated. Recognizing blood clot symptoms, understanding the associated risks, and knowing the available treatment options are crucial steps in managing and preventing this condition.
In conclusion, prevention and early treatment of blood clots are paramount. Educating yourself about the symptoms and risks, adhering to preventive measures, and seeking medical attention when needed can make a significant difference in your overall well-being. By taking these steps, you can protect yourself from the potentially life-threatening complications of blood clots and ensure a healthier future.