Venous Insufficiency (Varicose Veins and Spider Veins)
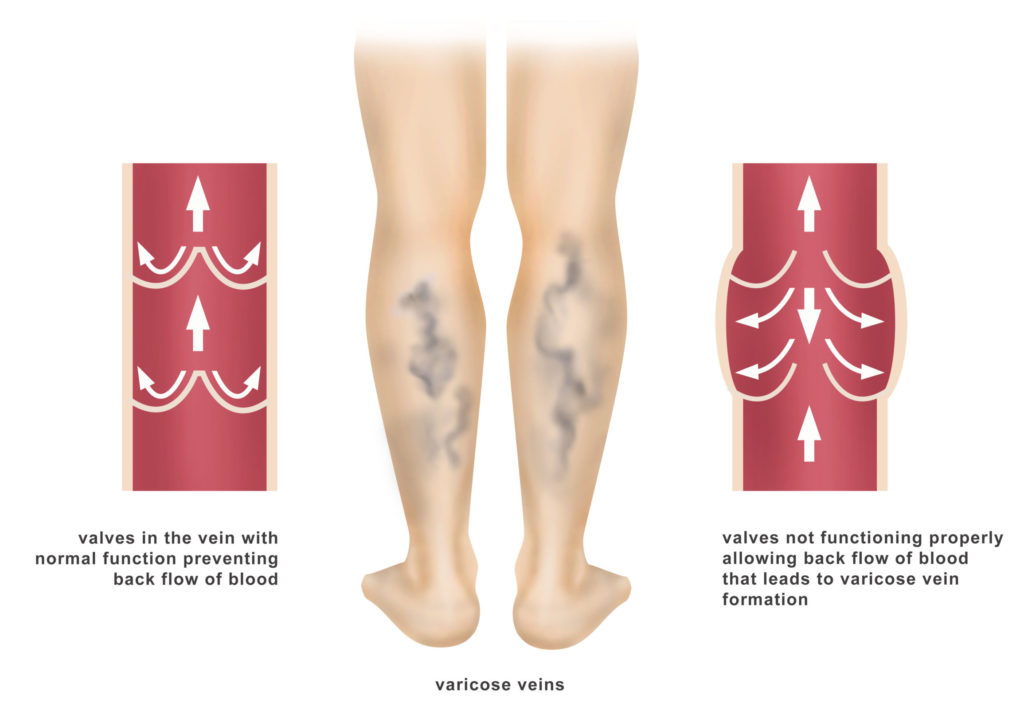
The veins are the blood vessels of the body that return blood from the arms, legs, and organs back to the heart. Normal circulation allows the arteries to carry blood from your heart to the rest of your body. In turn, your veins then carry your blood back to your heart. Standing and walking upright increases the pressure in the veins of your lower body. There are valves within the veins in your legs which are designed to prevent backflow of your blood. When these valves become impaired or when the forward flow of the blood through your veins is otherwise impaired, this condition is known as Venous Insufficiency.
Causes
- Age: As you get older, your veins can lose elasticity, causing them to stretch. The valves in your veins may become weak, allowing blood that should be moving toward your heart to flow backward.
- Blood pools in your veins, and your veins enlarge and become varicose. The veins appear blue because they contain deoxygenated blood, which is in the process of being recirculated through the lungs.
- Pregnancy: Some pregnant women develop varicose veins. Pregnancy increases the volume of blood in your body, but decreases the flow of blood from your legs to your pelvis. This circulatory change is designed to support the growing fetus, but it can produce an unfortunate side effect enlarged veins in your legs. Varicose veins may surface for the first time or may worsen during late pregnancy, when your uterus exerts greater pressure on the veins in your legs. Changes in your hormones during pregnancy also may play a role. Varicose veins that develop during pregnancy generally improve without medical treatment three to 12 months after delivery.
Risk factors
- Age: The risk of varicose veins increases with age. Aging causes wear and tear on the valves in your veins that help regulate blood flow. Eventually, that wear causes the valves to allow some blood to flow back into your veins where it collects instead of flowing up to your heart.
- Sex: Women are more likely to develop the condition. Hormonal changes during pregnancy, premenstruation or menopause may be a factor because female hormones tend to relax vein walls. Taking hormone replacement therapy or birth control pills may increase your risk of varicose veins.
- Family history: If other family members had varicose veins, there’s a greater chance you will too.
- Obesity:Being overweight puts added pressure on your veins.
- Standing or sitting for long periods of time. Your blood doesn’t flow as well if you’re in the same position for long periods.
- There’s no way to completely prevent varicose veins. But improving your circulation and muscle tone can reduce your risk of developing varicose veins or getting additional ones.
Symptoms
- Pain: The pain is described as a feeling of heaviness in the effected limb,dull ache, or throbbing pain. Pain is worsened by standing and relieved by rest and elevation. As symptoms progress the pain may become constant.
- Edema (swelling): As blood collects in your veins, swelling can occur. This occurs most prominently around the feet and ankles.
- Tingling: As blood pools in an area, this can cause a tingling sensation such as one would experience when a limb falls asleep. With venous insufficiency, this tingling may be accompanied with an itching sensation.
- Cramping: The lack of proper leg circulation can cause your legs to seize up and cramp.
- Skin discoloration: Also called stasis dermatitis or venous eczema, with prolonged pooling of blood in the legs and with the increased pressure blood leaks out of the vessels into the subcutaneous tissue and skin.
- Skin Ulcers: Skin ulcers can be caused with prolonged, severe venous insufficiency that leads to blood pooling particularly around the ankles. The ulcer(s) can appear as sore-like lesions on your skin. If left untreated, an ulcer can become an open wound.
Spider Veins
Spider veins consist of a network of small, colored veins appearing close to the surface of the skin. Typically caused by a backup of blood, spider veins can also occur due to injury, exposure to the sun, or changes in hormone levels; pregnancy can also be a contributing factor in the development of spider veins.
Spider veins often form web-like shapes beneath the surface of the skin and are red, blue, or purple appearing. Spider veins and varicose veins are related as both are swollen blood vessels which are visible through the skin with spider veins appearing closer to the surface of the skin and varicose veins being much larger, raised veins. Both most often appear in the lower extremities due to increased pressure on these veins. Obese people and those with occupations requiring long periods of sitting or standing are most susceptible to the development of varicose veins and spider veins.
Treatment
The most common treatment to remove spider veins is called Sclerotherapy. This modality of treatment for spider veins involves injecting a solution called sclerosant or foam sclerotherapy into the veins that will eventually cause the veins to close, making them disappear.
Varicose Veins
Varicose veins are not only unsightly, the veins which cause them have either damaged valves or no valves. This prevents the blood from traveling to your heart successfully causing the blood to build up in your legs.
Treatment
- Compression Hose: Prescription compression stockings or hose are elastic and will coax circulation in your veins by applying pressure at your ankle and lower leg to stimulate blood flow.
- Elevation: Elevate your legs to further help with your symptoms of swelling caused by the venous insufficiency
- Exercise: Exercise and keep your legs moving as exercise can also improve your circulation.
- Weight Loss: This can be helpful in the treatment of venous insufficiency for patients who are overweight.
- Radiofrequency Ablation: This is a minimally invasive procedure that uses radiofrequency energy (electricity) to heat, collapse and seal off the targeted blood vessels.
- Laser Ablation: Minimally invasive ultrasound-guided technique used for treating varicose veins using laser energy inserted into the vein to be treated. The laser light shines into the interior of the diseased vein.
- Glue Ablation: This is the latest minimally invasive technique where a sealent glue is injected into the vein under ultrasound guidance that seals the vein closed. This technique requires minimal use of local anesthetic and is not associated with any post procedure discoloration and can be done in the ambulatory setting in the office.
- Phlebectomy: Minimally invasive (nonsurgical) procedure to remove varicose veins on the surface of the leg. A small scalpel or needle is used make very small incisions near the varicose vein. A small phlebectomy hook is then used to remove the veins.
- Sclerotherapy: A modality of treatment for spider veins and varicose veins that involves injecting a solution called sclerosant or foam sclerotherapy into the veins that will eventually cause the veins to close, making them disappear.

