Deep vein thrombosis (DVT) is a medical condition that occurs when a blood clot forms in a deep vein. These clots usually develop in the lower leg, thigh, or pelvis, but they can also occur in the arm.
It is important to know about DVT because it can happen to anybody and can cause serious illness, disability, and in some cases, death. The good news is that DVT is preventable and treatable if discovered early.
Symptoms
Deep vein thrombosis signs and symptoms can include:
- Swelling in the affected leg. Rarely, there’s swelling in both legs.
- Pain in your leg. The pain often starts in your calf and can feel like cramping or soreness.
- Red or discolored skin on the leg.
- A feeling of warmth in the affected leg.
- Deep vein thrombosis can occur without noticeable symptoms.
- If you develop signs or symptoms of a pulmonary embolism that is a life-threatening complication of deep vein thrombosis seek immediate medical attention.
- The warning signs and symptoms of a pulmonary embolism include:
- Sudden shortness of breath
- Chest pain or discomfort that worsens when you take a deep breath or when you cough
- Feeling lightheaded or dizzy, or fainting
- Rapid pulse
- Coughing up blood
Risk Factors for DVT
Almost anyone can have a DVT. However, certain factors can increase the chance of having this condition. The chance increases even more for someone who has more than one of these factors at the same time.
Everyone Is at Risk. Some Factors Can Increase This Risk.
View the full infographic
Following is a list of factors that increase the risk of developing DVT:
- Injury to a vein, often caused by:
- Fractures,
- Severe muscle injury, or
- Major surgery (particularly involving the abdomen, pelvis, hip, or legs).
- Slow blood flow, often caused by:
- Confinement to bed
- (e.g., due to a medical condition or after surgery);
- Limited movement (e.g., a cast on a leg to help heal an injured bone);
- Sitting for a long time, especially with crossed legs; or
- Paralysis
- Increased estrogen, often caused by:
- Birth control pills
- Hormone replacement therapy, sometimes used after menopause
- Pregnancy, for up to 6 weeks after giving birth
- Certain chronic medical illnesses, such as:
- Heart disease
- Lung disease
- Cancer and its treatment
- Inflammatory bowel disease (Crohn’s disease or ulcerative colitis)
- Other factors that increase the risk of DVT include:
- Previous DVT or PE
- Family history of DVT or PE
- Age (risk increases as age increases)
- Obesity
- A catheter located in a central vein
- Inherited clotting disorders
Complications of DVT
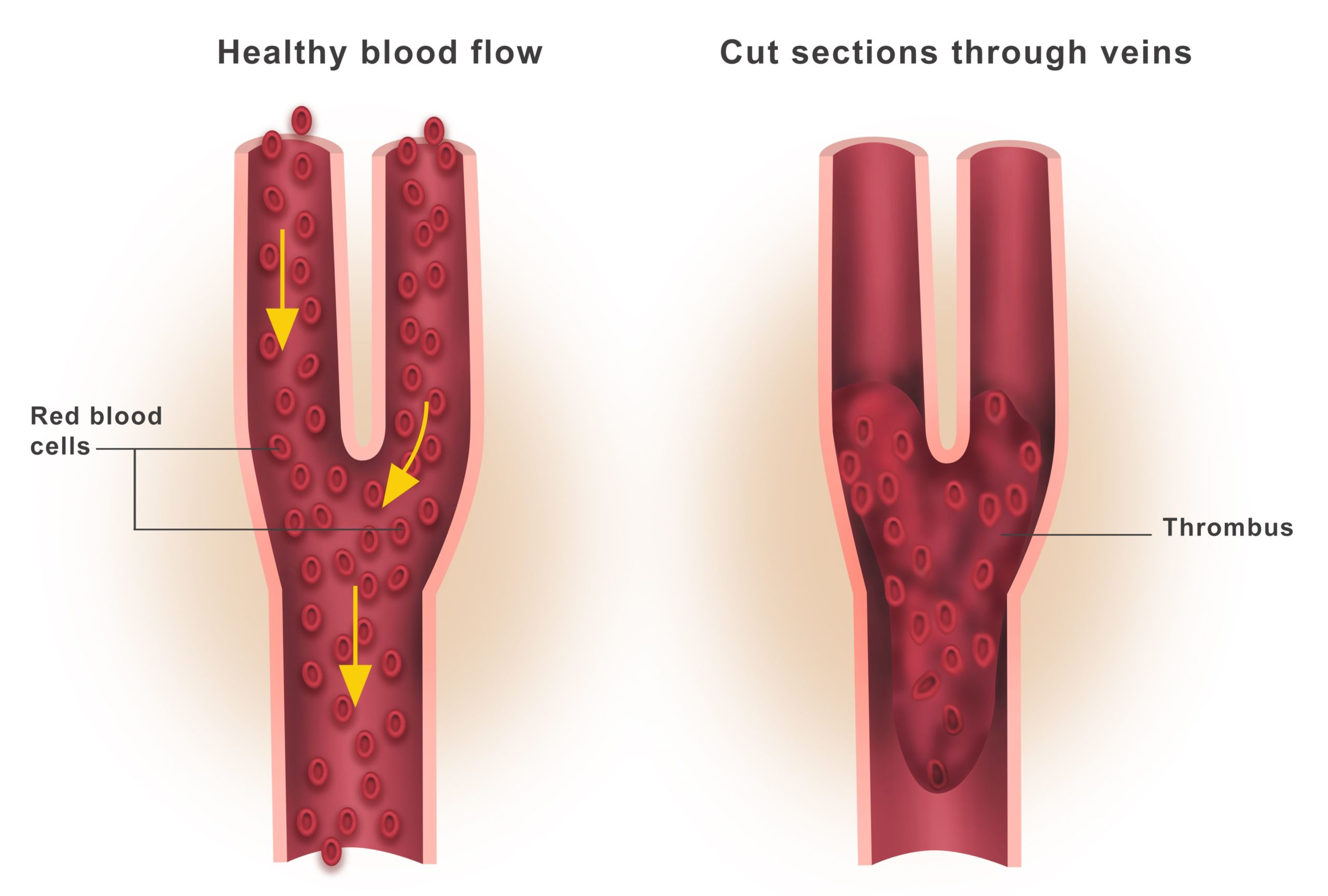
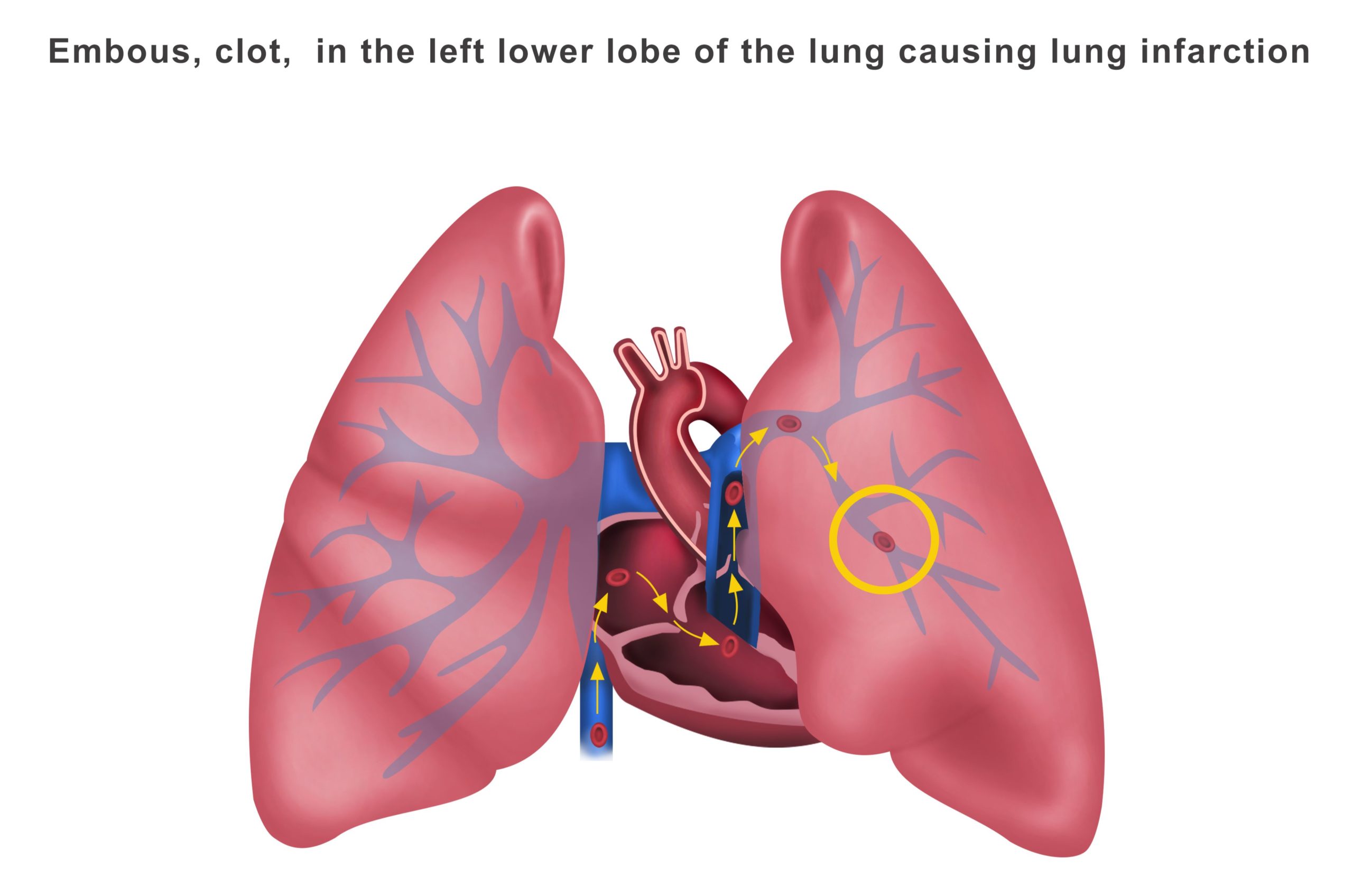
The most serious complication of DVT happens when a part of the clot breaks off and travels through the bloodstream to the lungs, causing a blockage called pulmonary embolism (PE). If the clot is small, and with appropriate treatment, people can recover from PE. However, there could be some damage to the lungs. If the clot is large, it can stop blood from reaching the lungs and is fatal.
In addition, nearly one-third of people who have a DVT will have long-term complications caused by the damage the clot does to the valves in the vein called post-thrombotic syndrome (PTS). People with PTS have symptoms such as swelling, pain, discoloration, and in severe cases, scaling or ulcers in the affected part of the body. In some cases, the symptoms can be so severe that a person becomes disabled.
For some people, DVT and PE can become a chronic illness; about 30% of people who have had a DVT or PE are at risk for another episode.
Preventing DVT
Move around as soon as possible after having been confined to bed, such as after surgery, illness, or injury.
If you are at risk for DVT, talk to your doctor about:
- Graduated compression stockings (sometimes called comedical compression stockings)
- Medication (anticoagulants) to prevent DVT.
When sitting for long periods of time, such as when traveling for more than four hours:
- Get up and walk around every 2 to 3 hours.
- Exercise your legs while you are sitting by:
- Raising and lowering your heels while keeping your toes on the floor
- Tightening and releasing your leg muscles
- Wear loose-fitting clothes.
You can reduce your risk by maintaining a healthy weight, avoiding a sedentary lifestyle, and following your doctor’s recommendations based on your individual risk factors.
Diagnosis
To diagnose deep vein thrombosis, your doctor will ask you about your symptoms. You’ll also have a physical exam so that your doctor can check for areas of swelling, tenderness or discoloration on your skin. Depending on how likely you are to have a blood clot, your doctor might suggest tests, including:
- Ultrasound. A wandlike device (transducer) placed over the part of your body where there’s a clot sends sound waves into the area. As the sound waves travel through your tissue and reflect back, a computer transforms the waves into a moving image on a video screen. A clot might be visible in the image.
- Sometimes a series of ultrasounds are done over several days to determine whether a blood clot is growing or to check for a new one.
- Blood test. Almost all people who develop severe deep vein thrombosis have an elevated blood level of a substance called D dimer.
- A dye is injected into a large vein in your foot or ankle. An X-ray creates an image of the veins in your legs and feet, to look for clots. However, less invasive methods of diagnosis, such as ultrasound, can usually confirm the diagnosis.
- CT or MRI scans. Either can provide visual images of your veins and might show if you have a clot. Sometimes these scans performed for other reasons reveal a clot.
Treatment
Deep vein thrombosis (DVT) treatment is aimed at preventing the clot from getting bigger and preventing it from breaking loose and causing a pulmonary embolism. Then the goal becomes reducing your chances of deep vein thrombosis happening again.
Deep vein thrombosis treatment options include:
- Blood thinners. Deep vein thrombosis is most commonly treated with anticoagulants, also called blood thinners. These drugs, which can be injected or taken as pills, decrease your blood’s ability to clot. They don’t break up existing blood clots, but they can prevent clots from getting bigger and reduce your risk of developing more clots.
- The injectable medications can be given as a shot under the skin or by injection into your arm vein (intravenous).
- You might receive an injectable blood thinner for a few days, after pills are started. Once the pill has thinned your blood, the injectable blood thinners are stopped.
- Other blood thinners can be given in pill form without the need for an injectable blood thinner.
- You might need to take blood thinner pills for three months or longer. It’s important to take them exactly as your doctor instructs because taking too much or too little can cause serious side effects.
- Clot busters(chemical and mechanical thrombolysis). If you have a more serious type of deep vein thrombosis or pulmonary embolism, or if other medications aren’t working, your doctor might prescribe drugs that break up clots quickly, called clot busters or thrombolytics.
- These drugs are either given through an IV line to break up blood clots or through a catheter placed directly into the clot. In addition mechanical devices are used to help break down the clot and remove it known as mechanical thrombolysis.
- If you can’t take medicines to thin your blood, you might have a filter inserted into a large vein, the vena cava is in your abdomen. A vena cava filter prevents clots that break loose from lodging in your lungs.
- Compression stockings. To help prevent swelling associated with deep vein thrombosis, these are worn on your legs from your feet to about the level of your knees.
- This pressure helps reduce the chances that your blood will pool and clot. You should wear these stockings during the day for at least two years, if possible.
FAQ
A condition where a clot partially or totally blocks the blood flow from a deep vein already present in the body, usually the vein in the leg. Nevertheless, this clot is a threat as it can move to the lungs causing pulmonary embolism.
Typically, deep vein thrombosis manifests the swelling of a single-sided leg at the early stage. Furthermore, swelling of the muscle of the calf or the thigh, a heavy or tight feeling, warmth, or an ache getting worse with standing or walking may also be noticed. Occasionally the skin might turn red or blue and at the same time, be more sensitive than usual. Under the situation that you in addition to this have a chest pain or sudden shortness of breath, it means that it is an emergency and you should get the help immediately.
First, Dr Ahmed Farah listens to your account of the events and he also performs a physical examination of your legs. He assesses the swelling, the color and temperature of the skin, and any areas of tenderness. Generally after this, he arranges a duplex ultrasound for you. It is a painless scan that shows how blood is flowing in the deep veins and if there is a clot that is obstructing the flow. If the case is not clear, he might also want to see other images and in some cases, he may suggest a blood test like D dimer.
Generally speaking, patients suffering from DVT are usually prescribed anticoagulants which will hinder further thrombus formation and the risk of the embolus going to the lungs will be lowered. In certain severe cases, doctors may also use minimally invasive procedures to mechanically remove or dissolve the clot, for example catheter based clot removal, when this is considered the safest option for you. Together with the length of the treatment, the amount of the drug and the therapy depend on your risk factors and whether it is your first clot or you have a repeated episode. The majority of people take the medication for three to six months and see their doctor in Dubai for regular checkups. A handful of patients who are at an extremely high-risk condition require prolonged protection and a detailed follow-up plan instead.
The risk of deep vein thrombosis can be reduced to a minimum through a perfect lifestyle which should include the taking of medication in the correct dose as instructed by the doctor, keeping physically active, and not sitting for long hours at a time. There are already a few things which could be done almost effortlessly like for instance regular daily walks, leg stretches in a long trip, staying in good shape and drinking enough water which are very helpful.
It is safe for most people to fly again after a deep vein thrombosis although timing is very important. Secondly Dr Ahmed Farah evaluates the presence of the clot, your overall well-being and the medication that you are taking at the moment and gives the go-ahead for the flight or not. He may put in a request for the use of compression stockings, be sure to drink plenty of water and walk up and down the aisle at regular intervals during the flight and at times he might also advise holding off on air travel until the risk has lessened further.

