What is carotid stenosis?
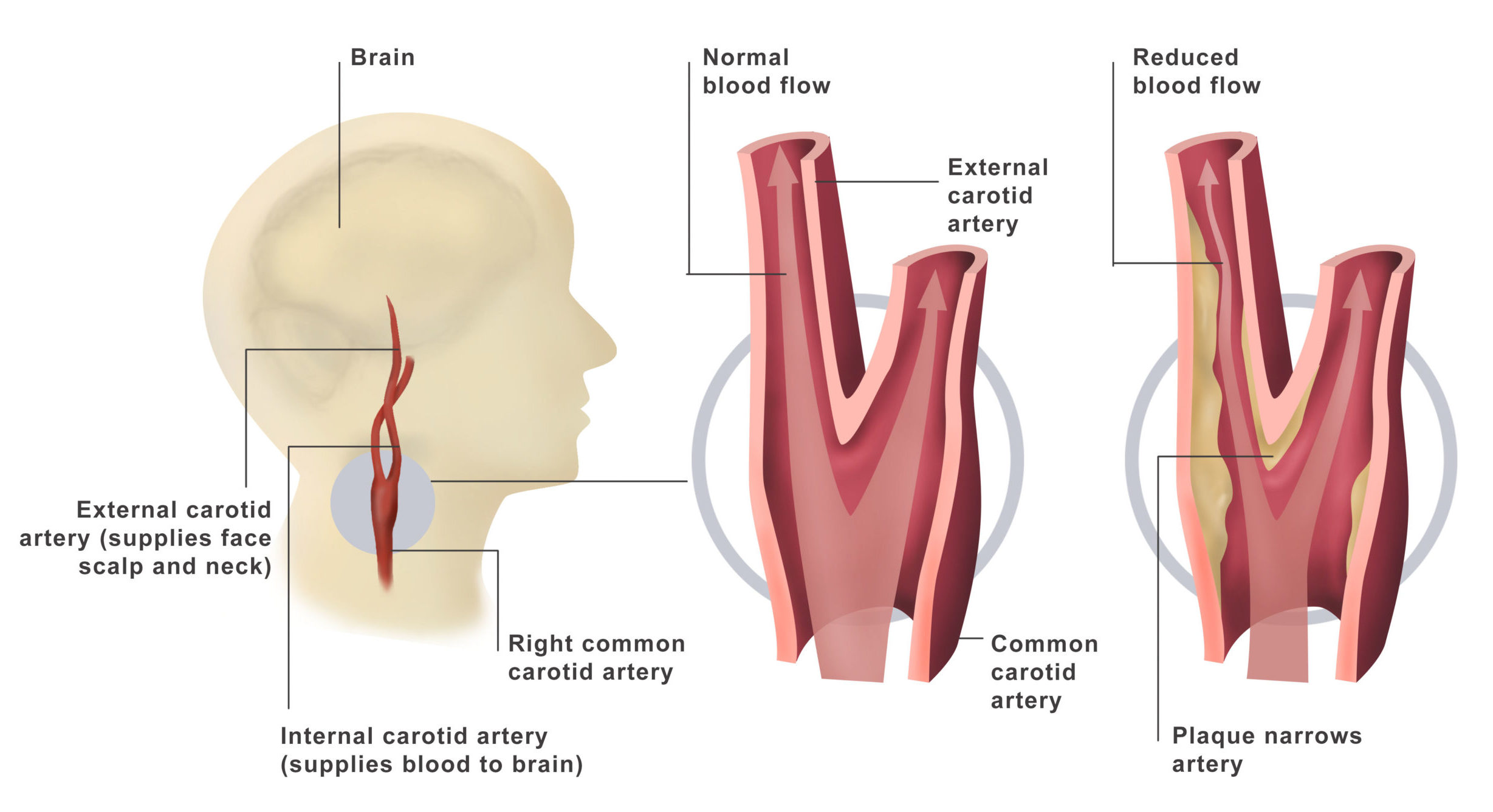
Carotid stenosis is a progressive narrowing of the carotid arteries in a process called atherosclerosis.
Normal healthy arteries are flexible and have smooth inner walls. As we age, hypertension and small injuries to the blood vessel wall can allow plaque to build up. Plaque is a sticky substance made of fat, cholesterol, calcium, and other fibrous material. Over time, plaque deposits inside the inner wall of the artery can form a large mass that narrows the lumen, the inside diameter of the artery. Atherosclerosis also causes arteries to become rigid, a process often referred to as “hardening of the arteries.”
Symptoms
In its early stages, carotid artery disease often doesn’t produce any signs or symptoms. The condition may go unnoticed until it’s serious enough to deprive your brain of blood, causing a stroke or TIA.
Signs and symptoms of a stroke or TIA include:
- Sudden numbness or weakness in the face or limbs, often on only one side of the body
- Sudden trouble speaking and understanding
- Sudden trouble seeing in one or both eyes
- Sudden dizziness or loss of balance
- Sudden, severe headache with no known cause
Risk factors
Factors that increase your risk of carotid artery disease include:
- High blood pressure. Excess pressure on artery walls can weaken them and make them more vulnerable to damage.
- Tobacco use. Nicotine can irritate the inner lining of your arteries. Smoking also increases your heart rate and blood pressure.
- Diabetes lowers your ability to process fats efficiently, placing you at greater risk of high blood pressure and atherosclerosis.
- High blood-fat levels. High levels of low-density lipoprotein cholesterol and high levels of triglycerides, a blood fat, encourage the accumulation of plaques.
- Family history. Your risk of carotid artery disease is higher if a relative has atherosclerosis or coronary artery disease.
- Arteries become less flexible and more prone to injury with age.
- Excess weight increases your chances of high blood pressure, atherosclerosis and diabetes.
Complications
Carotid artery disease causes about 10 to 20 percent of strokes. A stroke is a medical emergency that can leave you with permanent brain damage and muscle weakness. In severe cases, a stroke can be fatal.
Carotid artery disease can lead to stroke through:
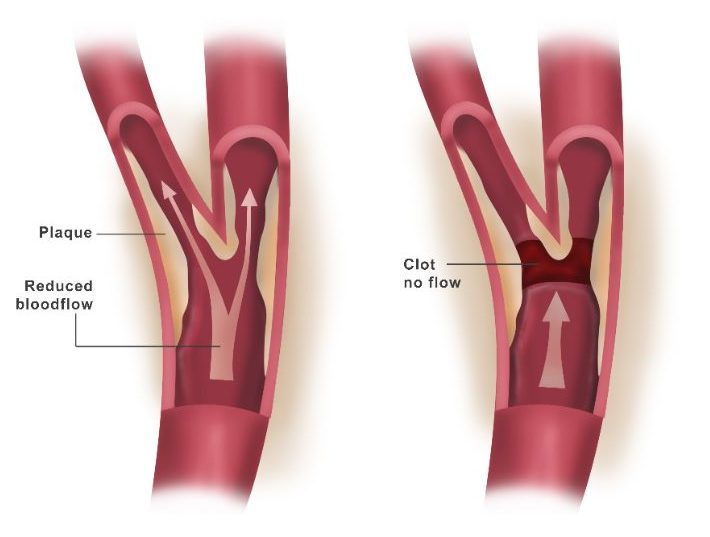
- Reduced blood flow. A carotid artery may become so narrowed by atherosclerosis that not enough blood is able to reach portions of your brain.
- Ruptured plaques. A piece of a plaque may break off and flow to smaller arteries in your brain. The plaque fragment may get stuck in one of these smaller arteries, creating a blockage that cuts off blood supply to part of your brain.
- Blood clot blockage. Some plaques are prone to cracking and forming irregular surfaces on the artery wall. Your body reacts as if to an injury and sends blood cells that help the clotting process to the area. The result can be a large clot that blocks or slows blood flow to the brain, causing a stroke.
Diagnosis
The following tests are used to aid in the diagnosis of carotid disease:
- Doppler ultrasound is a noninvasive test that uses reflected sound waves to evaluate blood flow through a vessel. The ultrasound probe is placed on the neck over the carotid arteries. This test will reveal how much blood is flowing through the artery and to what degree the artery has narrowed (i.e., 100%, 80%, 70%, etc.).
- Computed Tomography Angiography, or a CT angiogram, is a noninvasive X-ray that provides detailed images of anatomical structures within the brain. It involves injecting a contrast agent into the blood stream so that arteries of the brain can be seen. This type of test provides the best pictures of both blood vessels (through angiography) and soft tissues (through CT). It enables doctors to see the narrowed artery and to determine how much it has narrowed.
- Magnetic Resonance Angiography (MRA) of the neck is similar to the CT angiogram. Contrast dye is injected through an IV to illuminate blood vessels in the neck.
- Cerebral Angiogram is a minimally invasive test that uses X-rays and a contrast agent injected into the arteries through a catheter in the groin. It enables doctors to visualize all arteries in the brain.
Treatment
The goal of treatment is to reduce the risk of stroke. Treatment options vary according to the severity of the arterial narrowing and whether you are experiencing stroke-like symptoms or not.
Medications
People who have no symptoms or who have low-grade carotid stenosis of less than 50% are usually treated with medications. People who have a medical condition that would increase the risk of surgery also are likely to be treated with medication.
Medications include:
- Antiplatelet medications thin the blood and prevent clotting in the narrowed arteries, which allows blood to pass through more easily.
- Cholesterol-lowering statins help reduce plaque formation in atherosclerosis. Statins can reduce LDL “bad” cholesterol by an average of 25-30% when combined with a low-fat, low-cholesterol diet.
- Antihypertensive medications (diuretics, ACE inhibitors, angiotensin blockers, beta blockers, calcium channel blockers, etc.) help control and regulate blood pressure. Because high blood pressure is a major risk of stroke, regular blood pressure screenings are recommended.
Surgery
Surgical treatment is generally recommended for patients who have suffered one or more TIAs or strokes and who have a moderate to high grade of carotid stenosis. The aim of surgery is to prevent stroke by removing or reducing the plaque buildup and enlarging the artery lumen to allow more blood flow to the brain.
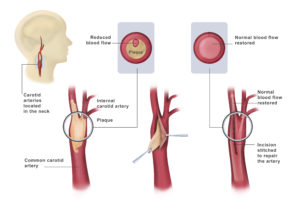
Carotid endarterectomy is an open surgery to remove the plaque. A skin incision is made in the neck and the carotid artery is located. Temporary clamps are placed across the artery above and below the area of stenosis to stop blood flow. During this time, the carotid artery on the other side of the neck carries blood flow to the brain. The surgeon makes an incision in the artery over the blocked area. The plaque buildup is peeled out and removed. The artery is then closed with tiny sutures and the clamps removed to allow blood flow to the brain.
 Carotid angioplasty / stenting is a minimally invasive endovascular procedure that compresses the plaque and widens the lumen of the artery. It is performed during an angiogram in a radiology suite. A flexible catheter is inserted in the femoral artery in the groin. It is guided through the blood stream past the heart, and into the carotid artery. Next, a small catheter with an inflatable balloon at the tip is positioned across the plaque. The balloon is opened to dilate the artery and compress the plaque against the artery wall. The balloon is then deflated and removed. Finally, a self-expanding mesh-like tube called a stent is placed over the plaque, holding open the artery.
Carotid angioplasty / stenting is a minimally invasive endovascular procedure that compresses the plaque and widens the lumen of the artery. It is performed during an angiogram in a radiology suite. A flexible catheter is inserted in the femoral artery in the groin. It is guided through the blood stream past the heart, and into the carotid artery. Next, a small catheter with an inflatable balloon at the tip is positioned across the plaque. The balloon is opened to dilate the artery and compress the plaque against the artery wall. The balloon is then deflated and removed. Finally, a self-expanding mesh-like tube called a stent is placed over the plaque, holding open the artery.
Angioplasty / stenting is typically indicated for select patients who
- have moderate to high-grade carotid stenosis greater than 70%;
- have other medical conditions that increase the risk of surgical complications;
- have recurrent stenosis; or
- have stenosis that was caused by prior radiation therapy.

