The section of the aorta that runs through the chest is called the thoracic aorta and, as the aorta moves down through the abdomen it is called the abdominal aorta.
What Is An Aortic Aneurysm?
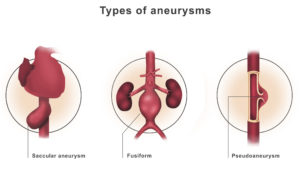
An aortic aneurysm is an abnormal enlargement or bulging of the wall of the aorta. An aneurysm can occur anywhere in the vascular tree. The bulge or ballooning may be defined as a:
- Fusiform: Uniform in shape, appearing equally along an extended section and edges of the aorta.
- Saccular aneurysm: Small, lop-sided blister on one side of the aorta that forms in a weakened area of the aorta wall.
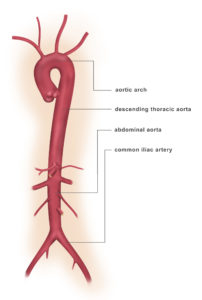
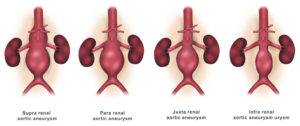
An aneurysm can develop anywhere along the aorta:
- Aneurysms that occur in the section of the aorta that runs through the abdomen (abdominal aorta) are called abdominal aortic aneurysms.
- Aortic aneurysms that occur in the chest area are called thoracic aortic aneurysms and can involve the aortic root, ascending aorta, aortic arch or descending aorta.
- Aneurysms that involve the aorta as it flows thru both the abdomen and chest are called thoracoabdominal aortic aneurysms.
Abdominal aortic aneurysms and thoracic aneurysm are not the only type of aneurysm. Aneurysms can develop in other blood vessels:
- Popliteal: an aneurysm in the artery behind the knee
- Renal: an aneurysm in the kidney; a very rare condition
- Visceral: an aneurysm in an internal organ and/or intestines
What are the Symptoms of Aortic Aneurysm?
Symptoms of a thoracic aortic aneurysm (affecting upper part of aorta in chest):
- Pain in the jaw, neck, upper back or chest
- Coughing, hoarseness or difficulty breathing
- Learn more about thoracic aortic aneurysm
Symptoms of an abdominal aortic aneurysm (affecting lower part of aorta in abdomen):
- Pulsating enlargement or tender mass felt by a physician when performing a physical examination
- Pain in the back, abdomen, or groin not relieved with position change or pain
Causes
Most aortic aneurysms occur in the part of your aorta that’s in your abdomen. Although the exact cause of abdominal aortic aneurysms is unknown, a number of factors may play a role, including:
- Tobacco use. Cigarette smoking and other forms of tobacco use appear to increase your risk of aortic aneurysms. Smoking can be damaging to the aorta and weaken the aorta’s walls.
- Hardening of the arteries (atherosclerosis). Atherosclerosis occurs when fat and other substances build up on the lining of a blood vessel. This condition may increase your risk of an aneurysm.
- High blood pressure. High blood pressure can increase your risk of abdominal aortic aneurysms as it can damage and weaken the aorta’s walls.
- Blood vessel diseases in the aorta. Abdominal aortic aneurysms can be caused by diseases that cause blood vessels to become inflamed.
- Infection in the aorta. Infections, such as a bacterial or fungal infection, may rarely cause abdominal aortic aneurysms.
- Trauma. Trauma, such as being in a car accident, can cause abdominal aortic aneurysms.
- Heredity. In some cases, abdominal aortic aneurysms could be hereditary.
Risk factors
Aortic aneurysm risk factors include:
- Age. Abdominal aortic aneurysms occur most often in people age 65 and older.
- Tobacco use. Tobacco use is a strong risk factor for the development of an abdominal aortic aneurysm and a higher risk of rupture. The longer you’ve smoked or chewed tobacco and the more cigarettes you smoked per day, the greater your risk.
- Being male. Men develop abdominal aortic aneurysms much more often than women do.
- Being white. People who are white are at higher risk of abdominal aortic aneurysms.
- Family history. People who have a family history of abdominal aortic aneurysms are at increased risk of having the condition.
- Atherosclerosis. Atherosclerosis is the buildup of fat and other substances that can damage the lining of a blood vessel that increases your risk of an aneurysm.
- Other aneurysms. People who have an aneurysm in another large blood vessel, such as the artery behind the knee or the thoracic aorta in the chest, may have a higher risk of developing an abdominal aortic aneurysm.
- High blood pressure. High blood pressure may increase your risk of developing an abdominal aortic aneurysm.
Complications
Tears in one or more of the layers of the wall of the aorta (aortic dissection) or a ruptured aortic aneurysm are the main complications of aortic aneurysms. A ruptured aortic aneurysm can lead to life-threatening internal bleeding. In general, the larger the aneurysm and the faster the aneurysm grows, the greater the risk of rupture.
Signs and symptoms that your aortic aneurysm has ruptured may include:
- Sudden, intense and persistent abdominal or back pain or chest pain, which can be described as a tearing sensation
- Pain that radiates to your back or legs
- Sweatiness
- Clamminess
- Dizziness
- Nausea
- Vomiting
- Low blood pressure
- Fast pulse
- Another complication of aortic aneurysms is the risk of blood clots. Small blood clots can develop in the area of the aortic aneurysm. If a blood clot breaks loose from the inside wall of an aneurysm and blocks a blood vessel elsewhere in your body, it can cause pain or block the blood flow to the legs, toes, kidneys or abdominal organs.
Diagnosis
Aortic aneurysms are often found during an examination for another reason. For example, during a routine exam, your doctor may feel a pulsating bulge in your abdomen, though it’s unlikely your doctor will be able to hear signs of an aneurysm through a stethoscope. Aortic aneurysms are also often found during routine medical tests, such as a chest X-ray or ultrasound of the heart(echocardiogram) or abdomen, sometimes ordered for a different reason.
To diagnose an aortic aneurysm, doctors will review your medical and family history and conduct a physical examination. If your doctor suspects that you have an aortic aneurysm, specialized tests can confirm it.
These tests might include:
Abdominal ultrasound or chest echocardiogram. This test is most commonly used to diagnose abdominal and thoracic aortic aneurysms. During this painless exam, you lie on your back on an examination table and a small amount of warm gel is applied to your abdomen chest. The gel helps eliminate the formation of air pockets between your body and the instrument the technician uses to see your aorta, called a transducer.
The technician presses the transducer against your skin over your abdomen or chest, moving from one area to another. The transducer sends images to a computer screen that the technician monitors to check for a potential aneurysm.
Computerized tomography (CT) scan. This painless test can provide your doctor with clear images of your aorta, and it can detect the size and shape of an aneurysm.
- During a CT scan, you lie on a table inside a doughnut-shaped machine. CT scanning generates X-rays to produce cross-sectional images of your body. Doctors may inject a dye into your blood vessels that helps your arteries to be more visible on the CT pictures (CT angiography).
Magnetic resonance imaging (MRI). An MRI is a painless imaging test that may be used to diagnose an aneurysm and determine its size and location.
- In this test, you lie on a movable table that slides into a tunnel. An MRI uses a magnetic field and pulses of radio wave energy to make pictures of your body. Doctors may inject a dye into your blood vessels to help your blood vessels to be more visible on images (magnetic resonance angiography).
Treatment
The goal of treatment is to prevent your aneurysm from rupturing. Generally, your treatment options are medical monitoring or surgery. The doctor’s decision depends on the size of the aortic aneurysm and how fast it’s growing.
Medical monitoring
If your aortic aneurysm is small and you’re not experiencing symptoms, the doctor may recommend medical monitoring, which includes regular appointments to make sure your aneurysm isn’t growing, and management of other medical conditions that could worsen your aneurysm. The doctor will also ask you about any signs or symptoms you may be experiencing that could be related to the aneurysm.
It’s likely the doctor will order regular imaging tests to check on the size of your aneurysm. Expect to have an abdominal ultrasound at least six months after your aneurysm is diagnosed and at regular follow-up exams after the first imaging test. The frequency of your imaging tests depends on the size of the aneurysm, whether the aneurysm is growing and how fast it’s growing.
Surgery
If you have an aortic aneurysm, surgery is generally recommended if your aneurysm is about 1.9 to 2.2 inches (about 5 to 5.5 centimeters) or larger. Doctors may also recommend surgery if the aneurysm is growing quickly. In addition, the doctor may recommend treatment if you’re experiencing symptoms such as stomach pain or you have a leaking, tender or painful aneurysm.
Surgery options may include:
Open abdominal surgery for abdominal aneurysms or open thoracic surgery for thoracic aneurysms. Open surgery to repair an aortic aneurysm involves removing the damaged section of the aorta and replacing it with a synthetic tube (graft), which is sewn into place. This procedure requires open surgery, and it will generally take you a month or more to fully recover.
Endovascular surgery. Endovascular surgery is a less invasive procedure used more frequently today to repair an aneurysm. Doctors attach a synthetic graft to the end of a thin tube (catheter) that’s inserted through an artery in your leg and threaded up into your aorta.
The graft is a woven tube covered by a metal mesh support that is placed at the site of the aneurysm and expanded. The graft is fastened in place with the metal mesh that frequently has small hooks or pins. The graft reinforces the weakened section of the aorta to prevent rupture of the aneurysm.
Recovery time is generally much shorter with this procedure than with open abdominal surgery, but endovascular surgery can’t be done in about 30 percent of people with an aneurysm. Discuss with the doctor whether you’re a candidate for this procedure. After endovascular surgery, you’ll need to have regular follow-up imaging tests to ensure that the graft isn’t leaking. Long-term survival rates are similar for both endovascular surgery and open surgery.
The options for treatment of your aneurysm will depend on a variety of factors, including location and size of the aneurysm, your age, and other existing conditions that may increase your risk of surgery or endovascular repair. The doctor will discuss with you the most appropriate treatment for you.

